Dental Implants have been around for decades as a means to supply a solution for the loss of teeth in adults (mostly). Over the past few decades, there has been a drastic increase in the number of people needing to have dental implant procedures done. This is mostly due to our lifestyle, and the high increase of sugar in our diets which has led to a higher rate of tooth loss in adults, and not just the elderly population.
When considering the restoration process, there are two common approaches: Cement restoration or screw retained. Which method to opt for is based on the patient’s needs and the professional opinion of the Doctor treating the case. The most obvious advantage a the screw retained method is that it enables a more favorable control on hygiene of the surrounding oral cavity as well as the implant itself. Moreover, if need be it is far easier to repair or replace a fractured crown. Instances, when cement restoration seems to be a better option is when there needs to be access to areas in the mouth such as the posterior, or when the hole is placed on the incisal edge.
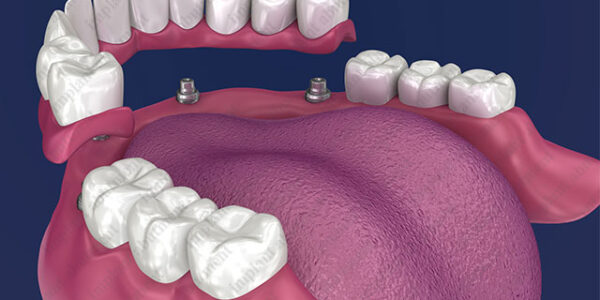
The most crucial procedure in a crown restoration is being able to produce an accurate mold/ impression of the section requiring restoration and delivering it to the laboratory thanks to the implant analogs. Once the area where the implant was inserted has had sufficient time to heal, it is possible to continue to the next step of the procedure. Healing time may vary from patient to patient, but should usually take between 2-3 weeks.
This is the stage where the implant analogs are introduced.
It is important to understand that the analogs have a pivotal role in the whole restoration process. In order to ensure precise and exact end results, it is of the greatest importance to make sure that premium quality implant analogs are used, including the materials used. Once the patient has healed from the initial implant placement, analogs are attached in the precise location where the final crown will be placed.
A mold/ impression is taken that will then be sent to the laboratory for further processing. Analogs assist laboratory technicians to position dental implants in the patient’s mouth by taking a mold, also known as impression coping. Once the mold is taken, the lab implant analogs are screwed into a position which helps create a final accurate mold for the final product.
The important role of the dental analog is to grant an exact point of reference for the lab technician to place and shape the abutments into place to later create a crown or bridge for the implant. This step in the process must be done correctly and with precision so that the mold that is then sent to the lab will ensure a satisfactory outcome, and naturally will affect the rest of the treatment for the patient.
It is extremely important to choose high-quality dental analogs since the design of the analog is specifically made to replicate the quality of the final implant (both internal and external) and that of the positioning in the patient’s mouth.
Which materials are best to use with Analogs?
In most cases analogs are made of stainless steel as it has been used since the 1900’s for medical purposes as well as replace biological tissue or create supporting structures for bones. Stainless steel is extremely resistant to corrosion when in contact with biological material.
However the use of titanium based analogs have become more popular recently in the world of dental implants and dentistry in general. The positive qualities that titanium has makes it a worthy material to use as it is stronger, approximately 50 percent lighter in weight, less rigid which creates less stress on the bone structure, has a higher tolerance to repetitive loads, less likely to provoke the immune system, is also resistant to corrosion and extremely biocompatible. This is why, nowadays we will most likely opt to use titanium based analogs rather than stainless steel, thus ensuring better compatibility as well as a longer life with lower risks of issues rising after the procedure has been completed.